دانشکده پزشکی
دانشگاه علوم پزشکی قم
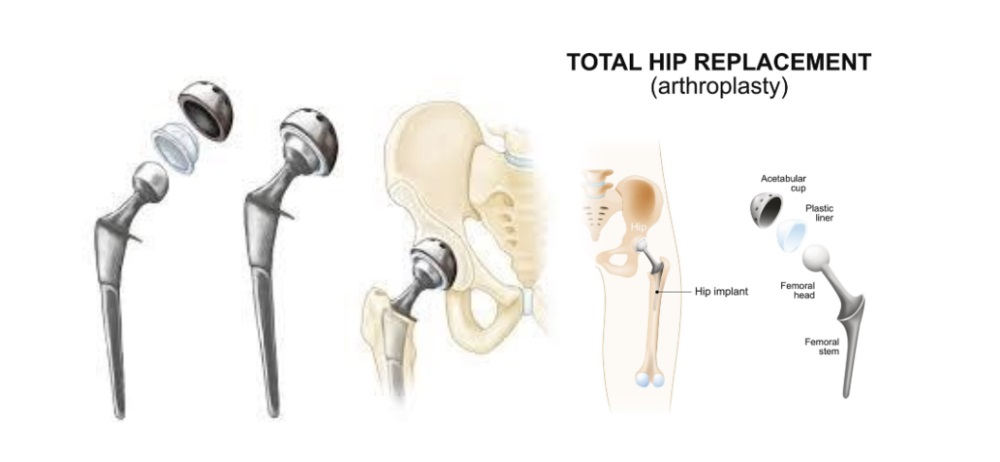
What is arthroplasty?
Arthroplasty is a surgical procedure to restore the function of a joint. A joint can be restored by resurfacing the bones. An artificial joint (called a prosthesis) may also be used.
Various types of arthritis may affect the joints. Osteoarthritis, or degenerative joint disease, is a loss of the cartilage or cushion in a joint, and is the most common reason for arthroplasty.
Why might I need arthroplasty?
Arthroplasty may be used when medical treatments no longer effectively relieve joint pain and disability. Some medical treatments for osteoarthritis that may be used before arthroplasty include:
- Anti-inflammatory medicines
- Pain medicines
- Limiting painful activities
- Assistive devices for walking (such as a cane)
- Physical therapy
- Cortisone injections into a knee joint
- Viscosupplementation injections (to add lubrication into the joint to make joint movement less painful)
- Weight loss (for obese people)
- Exercise and conditioning
People who have arthroplasty generally have substantial improvement in their joint pain, ability to perform activities, and quality of life.
Most joint surgery involves the hip and knee, with surgery on the ankle, elbow, shoulder, and fingers being done less often.
There may be other reasons for your healthcare provider to recommend arthroplasty. Please see hip replacement and knee replacement surgical procedures for more specific information
What are the risks of arthroplasty?
As with any surgical procedure, complications can happen. Some possible complications may include:
- Bleeding
- Infection
- Blood clots in the legs or lungs
- Loosening of prosthetic parts
Nerves or blood vessels in the area of surgery may be injured. This results in weakness or numbness. The joint pain may not be relieved by the surgery and/or complete function may not return.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
How do I prepare for arthroplasty?
- Your healthcare provider will explain the procedure to you and offer you the chance to ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- In addition to a complete medical history, your healthcare provider may perform a complete physical exam to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, and anesthetic agents (local and general).
- Tell your healthcare provider of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. It may be necessary for you to stop these medicines before the procedure.
- If you are pregnant or suspect that you are pregnant, you should notify your healthcare provider.
- You will be asked to fast for 8 hours before the procedure, generally after midnight.
- You may receive a sedative before the procedure to help you relax.
- You may meet with a physical therapist prior to your surgery to discuss rehabilitation.
- Arrange for someone to help around the house for a week or two after you are discharged from the hospital.
- Based on your medical condition, your healthcare provider may request other specific preparation.
What happens during arthroplasty?
Arthroplasty usually requires a stay in a hospital. Procedures may vary depending on your condition and your healthcare provider's practices.
Arthroplasty may be done while you are asleep under general anesthesia, or while you are awake under localized anesthesia. Your anesthesiologist will discuss this with you in advance.

Generally, arthroplasty follows this process:
- You will be asked to remove clothing and will be given a gown to wear.
- An intravenous (IV) line may be started in your arm or hand.
- You will be positioned on the operating table in a manner that provides the best access to the joint being operated on.
- A urinary catheter may be inserted.
- If there is excessive hair at the surgical site, it may be shaved off.
- The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- The skin over the surgical site will be cleansed with an antiseptic solution.
- The healthcare provider will make an incision in the area of the joint.
- The healthcare provider will repair or remove the damaged parts of the joint.
- The incision will be closed with stitches or surgical staples.
- A sterile bandage or dressing will be applied.
What happens after arthroplasty?
In the hospital
After the surgery you will be taken to the recovery room for observation. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room. Arthroplasty usually needs an in-hospital stay of several days.
It is important to begin moving the new joint after surgery. A physical therapist will meet with you soon after your surgery and plan an exercise rehabilitation program for you. Your pain will be controlled with medicine so that you can participate in the exercise program. You will be given an exercise plan to follow both in the hospital and after discharge.
You will be discharged home or to a rehabilitation center. In either case, your healthcare provider will arrange for continuation of physical therapy until you regain muscle strength and good range of motion.
At home
Once you are home, it will be important to keep the surgical area clean and dry. Your healthcare provider will give you specific bathing instructions. The stitches or surgical staples will be removed during a follow-up office visit.
Take a pain reliever for pain as recommended by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Notify your healthcare provider to report any of the following:
- Fever or chills
- Redness, swelling, bleeding, or other drainage from the incision site
- Increased pain around the incision site
- Numbness and/or tingling of the affected extremity
You may resume your normal diet unless your healthcare provider advises you differently.
You should not drive until your healthcare provider tells you to. Other activity restrictions may apply.
Making certain modifications to your home may help you during your recovery. These modifications include the following:
- Proper handrails along all stairs
- Safety handrails in the shower or bath
- Shower bench or chair
- Raised toilet seat
- Stable chair with firm seat cushion and firm back with two arms. This will allow your knees to be positioned lower than your hips
- Long-handled sponge and shower hose
- Dressing stick
- Sock aid
- Long-handled shoe horn
- Reaching stick to grab objects
- Firm pillows to raise the hips above the knees when sitting
- Removing loose carpets and electrical cords that may cause you to trip
Your healthcare provider may give you additional or alternate instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure







